Are Medicare ADRs Dead? What the New Documentation Requirements Really Mean for Hospice Providers
- 4compliancelady
- Nov 16, 2025
- 4 min read
Short answer: No, Medicare ADRs are definitely not dead. In fact, if you're a hospice provider hoping they've disappeared, we've got some news that might disappoint you. Additional Documentation Requests are alive and kicking in 2025, and understanding the current landscape is crucial for your agency's success.
Let's clear up the confusion and dive into what's really happening with Medicare ADRs and documentation requirements for hospice providers.
The Reality Check: ADRs Are Here to Stay
Despite wishful thinking from many providers, Medicare ADRs remain a core part of the oversight process. Recent guidance from March 2025 confirms that receiving an ADR is described as "a matter of when, not if" for hospice agencies. All agencies receive ADRs sooner or later, for a variety of reasons.
Think of ADRs as Medicare's way of double-checking your homework. They're not necessarily a red flag that something's wrong with your agency: they're simply part of Medicare's routine verification process to ensure that services billed were medically necessary and properly documented.

What Exactly Is an ADR?
An Additional Documentation Request is Medicare's formal way of asking you to provide specific documentation to support claims you've submitted. When Medicare sends an ADR, the letter will specify:
The exact claim(s) in question
The specific documents they need
Your submission deadline (usually 30-45 days)
Where and how to submit the documentation
The key thing to remember? This isn't a punishment: it's Medicare doing their due diligence to verify that everything checks out.
Who's Sending These ADRs?
Your ADR request can come from one of four different Medicare contractors, each with their own focus:
Medicare Administrative Contractors (MACs) are your most common source of ADRs. They process claims and handle routine documentation requests.
Recovery Audit Contractors (RACs) focus on identifying overpayments and underpayments in the Medicare system.
Unified Program Integrity Contractors (UPICs) investigate potential fraud and compliance issues: these tend to be more serious inquiries.
Supplemental Medical Review Contractors (SMRCs) conduct targeted medical reviews, often focusing on specific service types or patterns.
Knowing who's asking can help you understand the scope and urgency of the request.
The Two Types of ADRs You'll Encounter
Pre-payment ADRs happen before Medicare processes your claim for payment. These are essentially Medicare saying, "Hold up: we need to see some documentation before we pay this claim."
Post-payment ADRs occur after your claim has already been paid. These are part of routine post-payment review processes where Medicare circles back to verify that paid claims were appropriate.
Both types require the same level of attention and thoroughness in your response.
What's Changed: The Rules You Need to Know
Here's where things get interesting. Since January 1, 2019, CMS implemented specific rules to prevent ADR overload:
ADR Cycle Limits
Medicare now establishes a baseline annual ADR limit for each provider based on the number of Medicare claims paid in the previous 12-month period. This baseline is calculated as one-half of one percent of your total number of paid Medicare service types.
For example, if you had 1,000 paid Medicare claims last year, your baseline ADR limit would be 5 requests annually.
The Safety Net
If your calculated ADR cycle limit is less than 1, CMS rounds it up to at least 1 additional documentation request per 45 days until your annual ADR limit is reached. This ensures smaller providers aren't completely overwhelmed but still maintains oversight.
Documentation Requirements That Matter
When you receive an ADR, organization is everything. Here's what you need to gather:
All requested medical records (don't cherry-pick: send everything they ask for)
Care plans and physician certifications
Admission assessments and plans of care
Doctor's orders and supporting forms
Face-to-face encounter documentation (required before benefit periods)
Pro Response Tips
Put a copy of the ADR letter on top of your submission for easy processing
Ensure all pages are legible and properly sequenced
Include signature logs if necessary
Keep copies of everything you submit for your records
Submit by mail approximately 10 days before the deadline to ensure timely receipt
Remember: The due date is when Medicare must receive your documentation, not when you mail it.
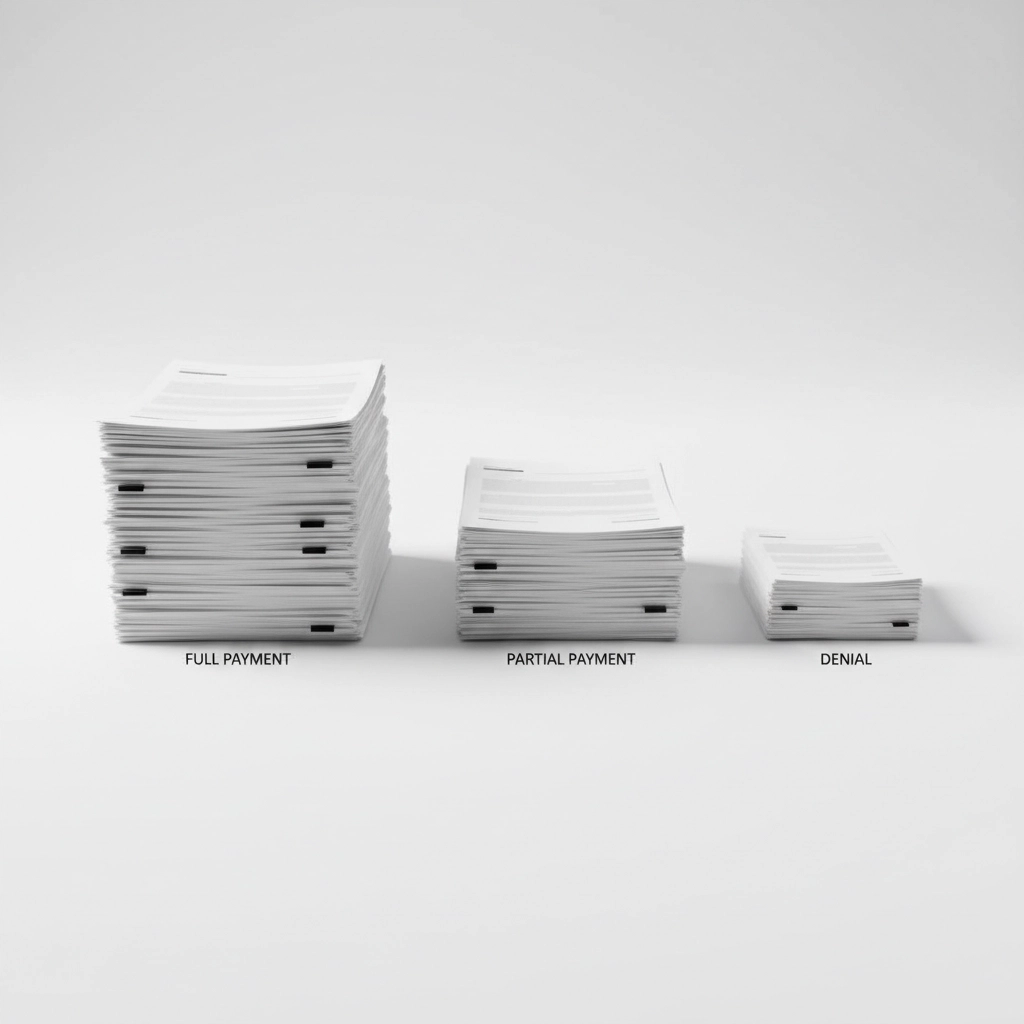
The Three Possible Outcomes
After you submit your ADR response, one of three things will happen:
Payment in full means Medicare is satisfied with your documentation and pays the claim as submitted.
Partial payment indicates some services were deemed appropriate while others weren't fully supported by the documentation.
Full denial means Medicare found the documentation insufficient to support the billed services.
If you receive a denial with reason code 56900 (indicating medical documentation wasn't received or wasn't received timely), you have 120 days to request a "56900 reopening" to have the documentation reviewed without going through the formal Medicare Appeals Process.
Beyond ADRs: Other Compliance Requirements
While ADRs get a lot of attention, they're just one piece of the compliance puzzle. Hospice providers must also navigate:
Hospice Quality Reporting Program (HQRP) requirements, with non-compliance resulting in up to 4% Medicare payment reductions
Face-to-face encounter requirements before each benefit period
Ongoing documentation standards that support medical necessity
What This Means for Your Agency
The bottom line? ADRs aren't going anywhere, but the rules around them provide some predictability. Rather than living in fear of the next ADR, focus on:
Maintaining excellent documentation practices from day one
Understanding your agency's ADR cycle limits based on your claims volume
Having systems in place for quick, organized ADR responses
Training staff on documentation requirements and ADR processes
Keeping current on Medicare requirements and changes
Moving Forward with Confidence
Medicare ADRs remain a reality for hospice providers in 2025, but they don't have to be a source of constant stress. With proper preparation, understanding of the process, and commitment to quality documentation, your agency can handle ADRs efficiently while focusing on what matters most: providing excellent patient care.
The key is shifting from reactive panic to proactive preparation. When you receive that next ADR (and you probably will), you'll be ready.
Need help strengthening your ADR response process or improving your documentation practices? Our team at ADR Prevention For You specializes in helping hospice providers navigate Medicare compliance challenges. Contact us today to learn how we can help protect your agency and streamline your compliance processes.

Comments